Key Facts About Tuberculosis
Key Facts About Tuberculosis

(updated March 20, 2020)
-
A total of 1.5 million people died from TB in 2018 (including 251,000 people with HIV). Worldwide, TB is one of the top 10 causes of death and the leading cause from a single infectious agent (above HIV/AIDS).
-
In 2018, an estimated 10 million people fell ill with tuberculosis(TB) worldwide. 5.7 million men, 3.2 million women and 1.1 million children. There were cases in all countries and age groups. But TB is curable and preventable.
-
In 2018, 1.1 million children fell ill with TB globally, and there were 205,000 child deaths due to TB (including among children with HIV). Child and adolescent TB is often overlooked by health providers and can be difficult to diagnose and treat.
-
In 2018, the 30 high TB burden countries accounted for 87% of new TB cases. Eight countries account for two thirds of the total, with India leading the count, followed by, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa.Multidrug-resistant TB (MDR-TB) remains a public health crisis and a health security threat. WHO estimates that there were 484 000 new cases with resistance to rifampicin – the most effective first-line drug, of which 78% had MDR-TB.Globally, TB incidence is acclerating due to COVID-19. This has been caused by the focus of drug manufacturers on COVID-19, the lack of clinical appointments available to diagnose TB, and a break in the supply chain for drugs.An estimated 58 million lives were saved through TB diagnosis and treatment between 2000 and 2018.Stopping TB from exploding epidemic over the next 10 months has become urgent as this is a "monster spreading" compared to Covid
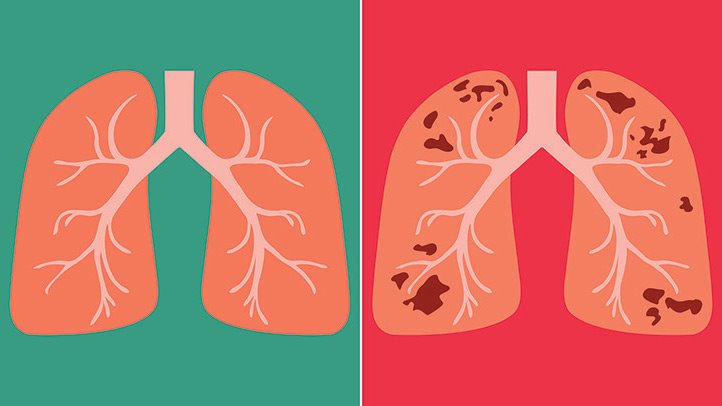
Tuberculosis (TB) is caused by bacteria (Mycobacterium tuberculosis) that most often affect the lungs. Tuberculosis is curable and preventable.
TB is spread from person to person through the air. When people with lung TB cough, sneeze or spit, they propel the TB germs into the air. A person needs to inhale only a few of these germs to become infected.
About one-quarter of the world's population has latent TB, which means people have been infected by TB bacteria but are not (yet) ill with the disease and cannot transmit the disease.
People infected with TB bacteria have a 5–15% lifetime risk of falling ill with TB. Persons with compromised immune systems, such as people living with HIV, malnutrition or diabetes, or people who use tobacco, have a higher risk of falling ill.
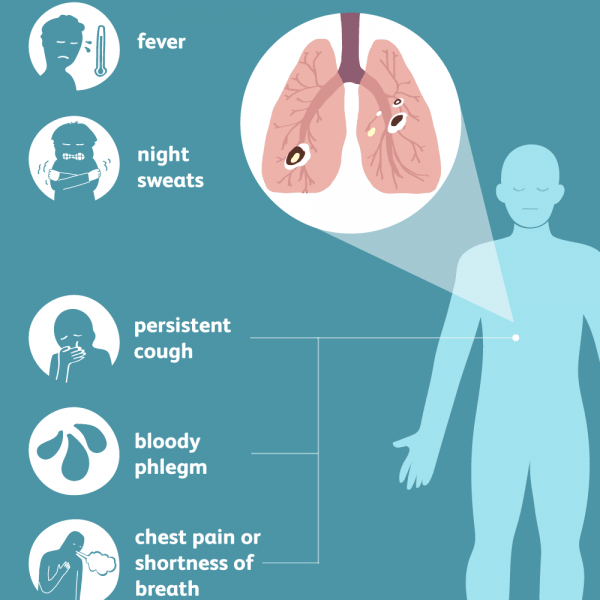
When a person develops active TB disease, the symptoms (such as cough, fever, night sweats, or weight loss) may be mild for many months. This can lead to delays in seeking care, and results in transmission of the bacteria to others. People with active TB can infect 5–15 other people through close contact over the course of a year. Without proper treatment, 45% of HIV-negative people with TB on average and nearly all HIV-positive people with TB will die.
Symptoms and diagnosis
Common symptoms of active lung TB are cough with sputum and blood at times, chest pains, weakness, weight loss, fever and night sweats. Many countries still rely on a long-used method called sputum smear microscopy to diagnose TB. Trained laboratory technicians look at sputum samples under a microscope to see if TB bacteria are present. Microscopy detects only half the number of TB cases and cannot detect drug-resistance.
The use of the rapid test Xpert MTB/RIF® has expanded substantially since 2010, when WHO first recommended its use. The test simultaneously detects TB and resistance to rifampicin, the most important TB medicine. Diagnosis can be made within 2 hours and the test is now recommended by WHO as the initial diagnostic test in all persons with signs and symptoms of TB.
Diagnosing multidrug-resistant and extensively drug-resistant TB (see Multidrug-resistant TB section below) as well as HIV-associated TB can be complex and expensive. In 2016, 4 new diagnostic tests were recommended by WHO – a rapid molecular test to detect TB at peripheral health centres where Xpert MTB/RIF cannot be used, and 3 tests to detect resistance to first- and second-line TB medicines.
Tuberculosis is particularly difficult to diagnose in children.
Treatment
TB is a treatable and curable disease. Active, drug-susceptible TB disease is treated with a standard 6-month course of 4 antimicrobial drugs that are provided with information and support to the patient by a health worker or trained volunteer. Without such support, treatment adherence is more difficult.
Between 2000 and 2018, an estimated 58 million lives were saved through TB diagnosis and treatment.
Who is most at risk?
Tuberculosis mostly affects adults in their most productive years. However, all age groups are at risk. Over 95% of cases and deaths are in developing countries.
People who are infected with HIV are 19 times more likely to develop active TB (see TB and HIV section below). The risk of active TB is also greater in persons suffering from other conditions that impair the immune system. People with undernutrition are 3 times more at risk. There were globally 2.3 million new TB cases in 2018 that were attributable to undernutrition.
1.1 million children (0–14 years of age) fell ill with TB, and 230,000 children (including children with HIV associated TB) died from the disease in 2018.
Alcohol use disorder and tobacco smoking increase the risk of TB disease by a factor of 3.3 and 1.6, respectively. In 2018, 0.83 million new TB cases worldwide were attributable to alcohol use disorder and 0.86 million were attributable to smoking.
Global impact of TB
TB occurs in every part of the world. In 2018, the largest number of new TB cases occurred in the South-East Asian region, with 44% of new cases, followed by the African region, with 24% of new cases and the Western Pacific with 18%.
In 2018, 87% of new TB cases occurred in the 30 high TB burden countries. Eight countries accounted for two thirds of the new TB cases: India, China, Indonesia, Philippines, Pakistan, Nigeria, Bangladesh and South Africa.
TB and HIV
People living with HIV are 19 (15-22) times more likely to develop active TB disease than people without HIV.
HIV and TB form a lethal combination, each speeding the other's progress. In 2018 about 251,000 people died of HIV-associated TB. In 2018, there were an estimated 862,000 new cases of TB amongst people who were HIV-positive, 72% of whom were living in Africa.
WHO recommends a 12-component approach of collaborative TB-HIV activities, including actions for prevention and treatment of infection and disease, to reduce deaths.
Multidrug-Resistant TB
Anti-TB medicines have been used for decades and strains that are resistant to one or more of the medicines have been documented in every country surveyed. Drug resistance emerges when anti-TB medicines are used inappropriately, through incorrect prescription by health care providers, poor quality drugs, and patients stopping treatment prematurely.
Multidrug-resistant tuberculosis (MDR-TB) is a form of TB caused by bacteria that do not respond to isoniazid and rifampicin, the 2 most powerful first-line anti-TB drugs. MDR-TB is treatable and curable by using second-line drugs. However, second-line treatment options are limited and require extensive chemotherapy (up to 2 years of treatment) with medicines that are expensive and toxic.
In some cases, more severe drug resistance can develop. Extensively drug-resistant TB (XDR-TB) is a more serious form of MDR-TB caused by bacteria that do not respond to the most effective second-line anti-TB drugs, often leaving patients without any further treatment options.
In 2018, MDR-TB remains a public health crisis and a health security threat. WHO estimates that there were 484,000 new cases with resistance to rifampicin – the most effective first-line drug – of which 78% had MDR-TB. The MDR-TB burden largely falls on 3 countries – India, China and the Russian Federation – which together account for half of the global cases. About 6.2% of MDR-TB cases had extensively drug-resistant TB (XDR-TB) in 2018.
Worldwide, only 56% of MDR-TB patients are currently successfully treated. In 2016, WHO approved the use of a short, standardized regimen for MDR-TB patients who do not have strains that are resistant to second-line TB medicines. This regimen takes 9–12 months and is much less expensive than the conventional treatment for MDR-TB, which can take up to 2 years. Patients with XDR-TB or resistance to second-line anti-TB drugs cannot use this regimen, however, and need to be put on longer MDR-TB regimens to which 1 of the new drugs (bedquiline and delamanid) may be added.
In July 2018, the latest evidence on treatment of drug-resistant TB was reviewed by an independent panel of experts convened by WHO. A rapid communication on key changes to recommendations for the treatment of drug-resistant TB has been issued by WHO, to be followed by the release of updated and consolidated WHO policy guidelines later in the year.
WHO also approved in 2016 a rapid diagnostic test to quickly identify these patients. Sixty-two countries have started using shorter MDR-TB regimens. By the end of 2018, 90 countries reported having introduced bedaquiline and 57 countries reported having introduced delamanid, in an effort to improve the effectiveness of MDR-TB treatment regimens.
Calendar




