How To Use Injectable Naloxone
 How To Use Injectable Naloxone
How To Use Injectable Naloxone
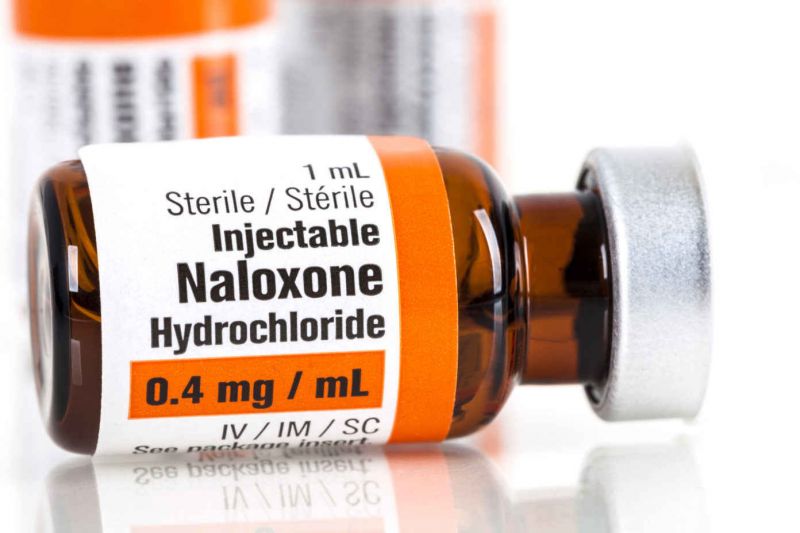
Naloxone
Naloxone (also called Narcan®) is an inexpensive, FDA-approved generic drug that works to reverse an opioid overdose, including fentanyl overdose, by restoring breath to unconscious overdose victims. Naloxone is not psychoactive, has no potential for misuse or abuse, and side effects are rare. Though all 50 states and the District of Columbia have passed legislation designed to improve layperson access to naloxone, these laws vary widely in scope.
How to Administer Naloxone
Naloxone is simple to administer, making it safe and easy for laypeople to use. Learn how to administer both nasal naloxone and naloxone by injection.
Benefits of Naloxone
- Naloxone programs prevent overdose fatalities. The Centers for Disease Control and Prevention (CDC) reports that, between 1996 and 2014, community-based overdose prevention programs trained and equipped more than 150,000 laypeople with naloxone, who successfully reversed over 25,000 opioid overdoses.
- Community-based naloxone distribution programs are widely supported. The American Medical Association, American Society of Addiction Medicine, Office of National Drug Control Policy, US Conference of Mayors, American Public Health Association, United Nations Office on Drugs and Crime, National Alliance of State and Territorial AIDS Directors, and many more support community-based naloxone programs.
- Naloxone is cost-effective. Providing take-home naloxone to people who use opioids – and their family, friends and caretakers – not only saves lives, it also saves money.
- Evidence shows that naloxone does not promote increases in drug use. Several studies have observed no serious adverse effects and no increase in risky behavior associated with naloxone availability. One study even found heroin use decreased after participation in a naloxone training program.
- Naloxone distribution programs connect people who use drugs to other necessary services. One study found that drug treatment entry increased after participation in a naloxone distribution and overdose prevention program.
Barriers to Naloxone Access
Naloxone should be available through a prescription to a family member, friend, or other person in a position to assist in an overdose, from community-based organizations like syringe access or overdose prevention programs, from pharmacies behind-the-counter, and from other critical intervention points such as jails and prisons, emergency rooms, and detox facilities among others.
There has been a political push to get naloxone in the hands of law enforcement and paramedics, but the first people on the scene of an overdose are often other people who use drugs and their peers or loved ones. This is why it’s important to prioritize community-based naloxone distribution, in addition to equipping conventional first responders.
Many states, however, only have access at one or very few of these intervention points. Moreover, very few states provide dedicated budget lines to support the cost of naloxone or staffing for community-based opioid overdose prevention programs, which means they are not able to serve nearly as many people as need naloxone. Virtually no jails or prisons provide naloxone upon release even though risk of a fatal overdose is nearly 130% greater in the two weeks after release compared to the general population.
In order to increase ease of access at various intervention points, naloxone should be made available over-the-counter and no longer classified as a prescription drug.
.mp4)




